Relevance: GS-2: Issues relating to the development and management of Social Sector/Services relating to Health, Education, Human Resources.
Key Phrases: Rural healthcare, Primary Health Centres, Sub Centres, Community Health Centres, Auxiliary Nursing Midwives, Lack of incentives, Urban-Rural divide, Government spending, Ayushman Bharat, National Rural Health Mission, Public-private partnerships, Neonatal mortality.
Why in News?
- Empty Hospitals in rural India and inadequate number of Doctors in Primary Health Centres is due to a lack of incentives extended to doctors prompting them not to work in rural health facilities is a matter of concern.
Status of Rural healthcare:
- More than two-thirds of Indians live in villages, but the healthcare facilities in these areas are yet to show the progress seen in urban areas.
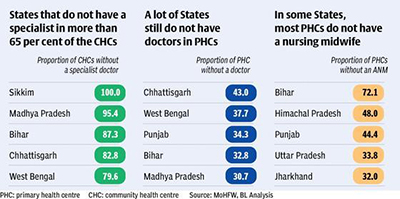
- In 2005, 17.49 per cent of the Primary Health Centres (PHCs) and Sub Centres (SC) functioned without Doctors, but the proportion of such centres will be as high as 21.83 per cent in 2021, according to rural health statistics of Ministry of Health and Family Welfare.
- Less than half the Community Health Centres (CHCs) had no specialist doctors in 2005, the vacancy was a whopping 67.96 per cent in 2021.

- Female health workers or Auxiliary Nursing Midwives (ANMs), the number of PHCs and Sub Centres devoid of them has jumped from 4.75 per cent in 2005 to 27.16 per cent in 2021.
- All the CHCs in Sikkim and 95 per cent in Madhya Pradesh are devoid of a specialist. 43.2 per cent of the PHCs in Chhattisgarh and 37.7 per cent in West Bengal also do not have a doctor.
- In Bihar, 72.12 per cent of Sub Centres has no female health worker who is supposed to manage them.
Why health facilities in rural India faces workforce crisis?
- Lack of incentives:
- Lack of incentives may be prompting Doctors to not work in rural health facilities.
- Urban-Rural divide:
- Health infrastructure is more in urban areas, so medical professionals are interested stay in urban areas.
- City-bred Doctors are not willing to serve in rural areas, many of which still lack of basic facilities like propre electricity and road connectivity etc.
- Indian medical education is geared to train Doctors to work only in tertiary care and specialised hospitals, so these medical professionals are not interested to stay in rural areas.
- Lack of incomes:
- Incomes in rural areas are less as compared to urban areas.
- Low government spending:
- Government spending on health is not even 2% of GDP.
- Health facilities are poor in rural areas.
- Lack of basic facilities:
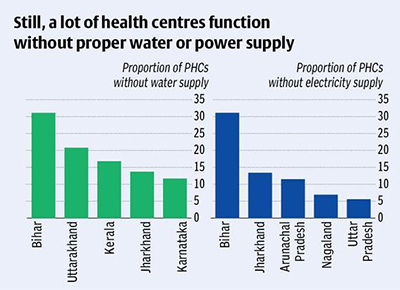
- Many health facilities are functioning without water or electricity supply.
- In Bihar, 31 per cent of the PHCs have neither water nor electricity supply.
- Twenty per cent of PHCs in Uttarakhand and 16 per cent in Kerala have no regular water supply.
Do you know?
- Neonatal mortality is three times in the poorest wealth quintile, highlighting inequalities experienced even by the young child.
- The lives of India’s poorest households are on average 7.6 years shorter than that of its richest 20 per cent households.
- The country faces a shortage of about six lakh doctors currently.
- India needs twice as many doctors as are available, three times as many nurses and four times as many paramedics.
- Catastrophic healthcare related expenditure pushes families into debt. More than 24% households in rural India and 18% of the population in urban areas have met their healthcare expenses through some sort of borrowings.
Government initiative to boost rural healthcare infrastructure:
- Ayushman Bharat Health Infrastructure Mission:
- It envisages increased investments in public health and other health
reforms to provide better access to health in rural areas by:
- Strengthening of Health and Wellness Centres in villages and cities for early detection of diseases.
- Addition of new critical care-related beds at district level hospitals.
- Support for Block Public Health Units (BPHU) in 11 high focus States
- Integrated district public health laboratories in all districts.
- It envisages increased investments in public health and other health
reforms to provide better access to health in rural areas by:
- National Rural Health Mission:
- Under the NRHM, support is provided to the States for ensuring a range of free services related to maternal health, child health, adolescent health, family planning, universal immunization etc.
- National Ambulance Service:
- Government of India in implementation of National Ambulance Service under NHM for free transportation to health facilities.
- This service is extended to remote and rural tribal areas also.
- States are free to place these Ambulances at a lower population norm or as per time to care approach so that these ambulances are easily accessible to all.
- ASHA workers:
- One of the key components of the NRH Mission is to provide every village in the country with a trained female community health activist – ASHA (Accredited Social Health Activist).
- An ASHA acts as the interface between the community and the public health system in rural India.
Key steps to strengthening rural healthcare infrastructure:
A few effective steps that, if implemented correctly, can empower rural healthcare systems and build healthy communities in the long-term.
- Long-term Public-Private Partnerships (PPP) to ensure healthcare
inclusion:
- PPP partnerships can transform the Indian rural healthcare system in more ways than one, with a long-term sustainable model.
- PPP can help overcome the limitations of financial, technological, educational, and human resources aspects.
- Government can frame policies around rural healthcare infrastructure, private players can ensure these are properly implemented.
- Such long-term partnerships increase access to healthcare particularly in difficult-to-reach rural areas as the private players’ expansive skills, experience and finance can help create innovative solutions.
- Establish an on-ground supervisory committee:
- An on-ground supervisory committee must be established to create a set of core and supplementary strategies to promote access to improved healthcare as well as oversee the implementation of rural healthcare initiatives.
- The committee is needed to revitalize rural health systems through effective monitoring of the rural health enhancement activities.
- On-going skill development and mentoring:
- Skill development courses and continuous learning programs for doctors and paramedical staff can help tackle the shortage of trained doctors in rural areas.
- Consistent upgradation of machines and training of paramedical staff:
- Rural areas lack essential facilities such as the latest medical equipment and trained medical staff to man the equipment.
- Training workshops for nurses and para medical staff on effective handling, operating and managing these equipment is also vital.
Way forward:
- Medical institutions should motivate the upcoming doctors to provide their education and services in rural parts of the country as well as remind them that the profession revolves around saving lives.
- The issue of lack of doctors for rural areas can also be addressed to a certain extent by reintroducing “Licentiate Medical Practitioners”.
- The government should create a framework for the right staffing, duration and think about the incentives and career paths of doctors and all levels of staff to work in a rural health centre.
- Union Government and the Medical Council of India should formulate a policy regarding the compulsory service in rural area for a certain duration to be rendered by the Doctors who are trained in government institutions.
Source: The Hindu BL
Mains Question:
Q. Rural India is struggling with a ‘Missing Doctors Syndrome’. Discuss and suggest measures to deal with the problem.