Context
The Health Ministry and the Insurance Regulatory and Development Authority of India (IRDAI) are collaborating to enhance the accessibility and affordability of quality healthcare in India. As part of this initiative, they are launching the National Health Claim Exchange (NHCX), a digital platform designed to streamline interactions between insurance companies, healthcare service providers, and government insurance scheme administrators. The primary aim is to reduce out-of-pocket expenses for patients while ensuring swift access to healthcare.
Functionality of the NHCX
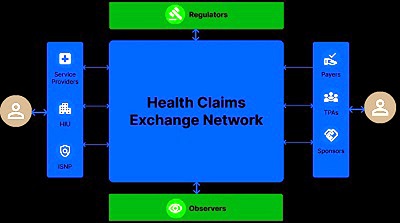
The NHCX is envisioned as a central gateway for the exchange of claims-related information among stakeholders in the healthcare and health insurance ecosystem. It is expected to enable seamless interoperability in health claims processing, thereby increasing efficiency and transparency in the insurance industry. According to the Health Ministry, this will benefit both policyholders and patients by simplifying the claims process.
Integration and Benefits
S. Prakash, MD & CEO designate of Galaxy Health and Allied Insurance Company Limited, highlights that the insurance industry is ready to support the NHCX implementation. The platform aims to facilitate streamlined interactions between hospitals and insurers, creating a seamless, paperless, and secure contractual framework. By acting as a centralized hub for all health claims, the NHCX will significantly reduce the administrative burden on hospitals, which currently have to manage multiple portals for various insurers. Twelve insurance companies and one Third Party Administrator (TPA) have already completed integration with the NHCX.
Cashless Claims Processing
A significant feature of the NHCX is its impact on cashless claims. The insurance authority has mandated that all cashless claims must be processed within three hours of receiving discharge authorization from the hospital. Insurance providers have been given a deadline of July 31 to implement the necessary systems and processes to ensure compliance with this directive, aiming to facilitate smoother and faster claims processing.
Incentives for Digital Adoption
To encourage the adoption of digital health transactions and the digitization of patient health records, the National Health Authority has introduced the Digital Health Incentive Scheme (DHIS). Starting January 2023, hospitals are eligible for financial incentives for each insurance claim transaction processed through the NHCX. The incentives are set at ₹500 per claim or 10% of the claim amount, whichever is lower, as per a Health Ministry note. This initiative is designed to promote the digitization of health records and streamline claim processes.
Rationale for NHCX
Health insurance is a critical strategy for providing healthcare services and reducing the high out-of-pocket expenditure that burdens individuals. A paper titled "Health Insurance Coverage in India: Insights for National Health Protection Scheme" emphasizes the importance of health insurance in mitigating these expenses. The paper notes that hospitalization cases are highest for those with private insurance in both rural and urban areas. The NHCX aims to standardize and improve the interoperability of health claims, facilitating a seamless exchange of data, documents, and images between payers and providers. Industry experts believe that through uniform data presentation and central validation of claims data, the platform can bring about a more standardized approach to healthcare pricing.
Challenges and Solutions
Despite the potential benefits, several challenges remain. Health insurance contributes to approximately 29% of the total general insurance premium income in India. The primary challenge is improving the relationship between hospitals and insurance companies. This push towards digitization requires active involvement from both parties, necessitating IT system upgrades and enhanced workforce training. Issues such as discharge delays and miscommunication between hospitals and insurers further complicate matters. Building trust among policyholders hinges on the delivery of efficient services.
Dr. Prakash acknowledges that while the NHCX portal aims to streamline the claims process by bringing all stakeholders onto one platform, reducing claim times, and standardizing procedures, issues like data breaches must be effectively managed. Despite these challenges, the NHCX stands as an ongoing benefit for all involved, facilitating smoother operations within the healthcare space.
Conclusion
The National Health Claim Exchange (NHCX) represents a significant step towards achieving IRDAI’s objective of "Insurance for All by 2047." By creating a centralized, digital platform for health claims, it promises to enhance efficiency, transparency, and trust in the health insurance ecosystem. While challenges such as IT system upgrades and data security remain, the collaborative efforts of the Health Ministry and IRDAI, supported by industry stakeholders, are poised to bring about meaningful improvements in healthcare access and affordability in India.
|
Probable Questions for UPSC Mains Exam
|
Source – The Hindu