Context:
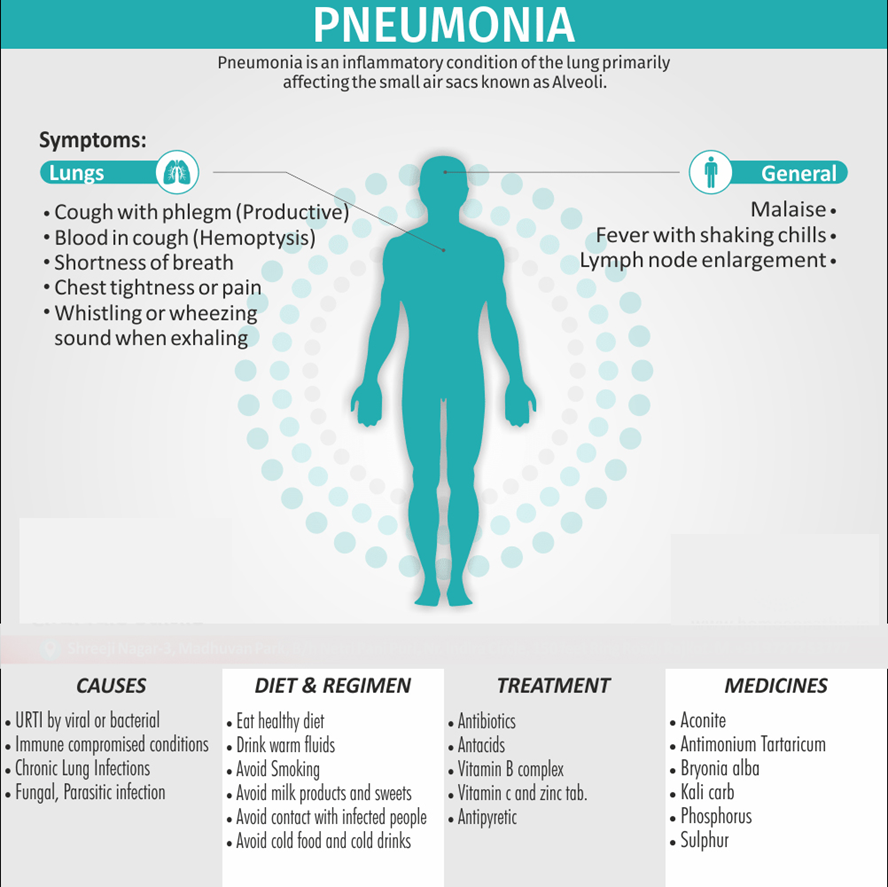
Pneumonia, a potentially fatal respiratory infection, remains a global health challenge, particularly in low- and middle-income countries where access to healthcare is limited. Despite significant medical advancements, pneumonia continues to be one of the leading causes of death, contributing to substantial morbidity and mortality, especially among vulnerable populations such as children, the elderly, and those with chronic conditions. In India, the burden of pneumonia is particularly heavy, with millions of lives affected annually.
About Pneumonia: First identified over a century ago by microbiologists Louis Pasteur and George Sternberg, Streptococcus pneumoniae has since evolved into one of the most persistent and lethal pathogens.
- Global Burden: Each year, pneumonia remains among the leading causes of death globally. In India, it has a particularly dire impact, especially on children under five. According to estimates, over 127,000 children in India die from pneumonia annually, accounting for 14% of the deaths in this age group.
- World Pneumonia Day: Observed on 12 November, World Pneumonia Day serves as a reminder of the urgent need for targeted intervention and prevention efforts to reduce pneumonia-related fatalities.
Vulnerable Populations and Regional Disparities:
- Socioeconomic Factors: Vulnerability to pneumonia is exacerbated by poverty, overcrowded living conditions, and limited access to healthcare and nutrition. These factors are particularly prominent in rural areas.
- Impact on Children: In states like Madhya Pradesh and Uttar Pradesh, pneumonia incidence rates among children exceed 500 cases per 1,000 children, reflecting the acute burden in these regions. Pneumonia is responsible for 44% of deaths in children under five globally.
- Environmental and Behavioral Factors: Poor air quality in urban areas and reliance on solid fuels for cooking contribute significantly to the prevalence of respiratory infections, further increasing the risk of pneumonia, particularly among children.
Health Infrastructure Challenges:
- Limited Vaccine Coverage: Vaccination coverage remains inconsistent due to logistical problems and lack of awareness. While the pneumococcal conjugate vaccine (PCV) has been included in the Universal Immunization Programme (UIP) since 2017, its reach remains limited, especially in rural and underserved areas.
- Shortage of Skilled Health Workers: A shortage of skilled medical professionals, such as pediatricians and general practitioners, along with insufficient medical supplies, including oxygen therapy units, hinders effective treatment, particularly in rural regions.
- Antimicrobial Resistance (AMR): The growing problem of AMR compounds the issue by making pneumonia treatment more difficult and expensive. Resistant pathogens lead to longer hospital stays and require costly broad-spectrum antibiotics, further driving up healthcare costs and mortality rates.
Socioeconomic Impact of Pneumonia:
- Direct Healthcare Costs: Treating pneumonia, particularly severe cases that require hospitalization or ventilator support, incurs high direct costs. Studies suggest that the cost of treating ventilator-associated pneumonia (VAP) can be INR 249,199, while the cost of treating community-acquired pneumonia (CAP) varies between INR 5,575 in government hospitals to INR 210,862 in private hospitals.
- Indirect Costs: Indirect costs, such as loss of productivity, caregiver time, and additional financial strain on families, contribute to a significant economic toll. Patients with CAP may miss an average of 16 workdays if hospitalized, and caregivers, particularly in public hospitals, experience significant work absences.
- Regional Variations: Studies show that the economic burden of pneumonia varies across regions. For example, in Pune, the direct treatment costs are higher, whereas in Chennai, indirect costs related to caregiving and lost productivity are more significant. These variations are further exacerbated by the limited availability of health insurance coverage for pneumonia treatment.
Pneumococcal Vaccination: A Key Solution:
- Pneumococcal Conjugate Vaccine (PCV): In 2017, India introduced the PCV as part of the UIP, with 83% of infants being vaccinated by 2022. This effort has contributed to a decrease in the under-five mortality rate from 45 per 1,000 live births in 2014 to 32 per 1,000 in 2020. The introduction of PCV has had a significant positive impact on reducing pneumonia-related deaths among children.
- Adult Pneumococcal Vaccination: While much focus has been on vaccinating children, pneumonia remains a leading cause of death among the elderly as well. However, India’s adult vaccination rates, particularly for pneumococcal vaccines, remain alarmingly low. A systematic review from 2010 to 2020 found that India had one of the lowest adult pneumococcal vaccination rates in the Indo-Pacific region. For adults aged 45 and above, pneumococcal vaccination coverage was found to be just 1.5%.
- Barriers to Vaccination: Several factors contribute to the low vaccination rate among adults, including a lack of national vaccination guidelines, low health awareness, and economic constraints. Urban, wealthier individuals with more years of schooling are more likely to receive vaccinations. This highlights the need for increased public health education and improved access to vaccines for older adults.
Economic Impact of Pneumonia on Households:
- High Treatment Costs: For families living in rural areas, the direct and indirect costs of pneumonia treatment are often unaffordable. Many families, particularly those with children, rely on external financial support to cover medical expenses.
- Work Absences and Caregiving Burden: As mentioned earlier, pneumonia treatment requires significant caregiver involvement, with most patients needing support from family and friends during recovery. The absence of caregivers from work, especially in public healthcare settings, places additional strain on families.
Policy Recommendations for Addressing Pneumonia:
- Expansion of Vaccination Programs: Mass vaccination campaigns for both children and adults are critical to reducing the incidence of pneumonia. In particular, increasing adult pneumococcal vaccination rates through national guidelines and awareness campaigns can significantly lower pneumonia-related mortality in older populations.
- Improvement in Health Infrastructure: Strengthening the healthcare infrastructure, particularly in rural areas, is essential. This includes improving the availability of skilled healthcare workers, medical consumables like oxygen therapy, and ensuring that antibiotics remain effective in treating pneumonia.
- Reducing Environmental Risks: Addressing air quality and transitioning to cleaner cooking technologies would reduce the incidence of pneumonia, especially in children. Policies to mitigate indoor air pollution, such as promoting clean energy and proper ventilation in homes, would go a long way in reducing pneumonia risk.
- Socioeconomic Support: Given the economic burden on families, it is essential to invest in social safety nets, insurance coverage, and financial support for pneumonia patients, particularly in low-income households.
Conclusion:
India has made strides in tackling pneumonia, particularly through the introduction of the PCV and increased immunization efforts. However, challenges remain, particularly in rural areas where vaccination coverage is still low, and healthcare infrastructure is inadequate. A comprehensive approach that includes expanding vaccination programs, improving healthcare infrastructure, and addressing environmental and socioeconomic factors is essential to reducing the impact of pneumonia in India. Investing in these areas will not only reduce the human toll but also alleviate the significant economic burden of this preventable disease.
|
Probable questions for UPSC Mains exam: Discuss the challenges and successes of India’s efforts to vaccinate children under five years old against pneumonia. How effective has the introduction of the pneumococcal conjugate vaccine (PCV) been in preventing pneumonia deaths among children? |