Over the last decade, India has made substantial progress in reforming its health financing system, with a specific focus on reducing out-of-pocket expenditures (OOPE) that burden a large section of the population. Research studies suggest that between 3% to 7% of Indian households are pushed below the poverty line annually due to OOPE in health, especially in rural and poorer states. Addressing this issue has become a key policy priority, as seen in the latest release of the National Health Account (NHA) estimates for 2020-21 and 2021-22 by the Government of India on 25th September 2024.
While the country has made great strides, challenges still remain as it aims to meet the National Health Policy (NHP) 2017 target of 2.5% of GDP worth of government expenditure in health by 2025.
Significant Decline in Out-of-Pocket Expenditure (OOPE):
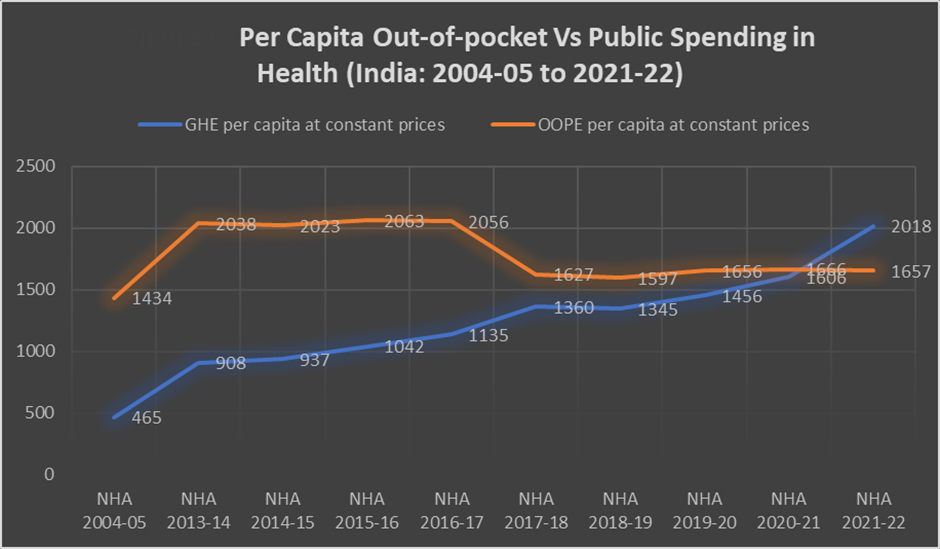
The latest NHA estimates reveal a dramatic decline in OOPE over the past decade. In 2013-14, OOPE accounted for 64.2% of total health expenditure, but by 2021-22, this figure had fallen to 39.4%. This reduction represents a pivotal shift in the financial burden from individuals to the government, driven by increased government investments in health and the introduction of multiple health programs. This trend is expected to continue, although 39.4% remains a substantial figure that calls for continued policy intervention.
· OOPE dropped from 64.2% in 2013-14 to 39.4% in 2021-22
· The decline has been part of an ongoing trend throughout the decade, accelerated by increased health spending during the COVID-19 pandemic.
Increase in Government Health Expenditure (GHE):
One of the major drivers behind the reduction of OOPE is the sharp rise in Government Health Expenditure (GHE). Between 2013-14 and 2021-22, GHE grew from 28.6% to 48.0% of total health expenditure. This marks a historic moment in India’s health policy, where public spending now surpasses OOPE for the first time.
· Government health spending rose from 28.6% in 2013-14 to 48.0% in 2021-22.
· The pandemic-induced surge in health allocations contributed significantly to this rise, though the upward trend had begun before the pandemic.
This shift signifies a more equitable health financing system, although there remains a considerable gap between India's current GHE and the NHP 2017 goal of reaching 2.5% of GDP by 2025. The challenge is to maintain the upward momentum in health spending even as the immediate effects of the pandemic subside.
Total Health Expenditure (THE) and Government Initiatives:
While public health spending increased, Total Health Expenditure (THE) as a percentage of GDP decreased over the last decade. This paradoxical trend is due to the growing share of government health spending, which has lessened the financial burden on families.
Despite these gains, OOPE still accounts for 39.4% of total health expenditure, highlighting a persistent issue. India still faces challenges in reducing this figure further, especially to achieve its target by 2025.
Government Programs Contributing to OOPE Reduction:
1. Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY): Launched in 2018, AB-PMJAY has become a cornerstone of India’s healthcare system, offering free secondary and tertiary care to vulnerable populations. By 2024, it had facilitated 69 million hospital admissions across the country.
2. Ayushman Bharat Health and Wellness Centres (AAMs): These centers focus on delivering comprehensive primary healthcare at the grassroots level, especially in rural areas. As of 2024, over 1.75 lakh functional AAMs had been established, providing services such as non-communicable disease management, maternal and child healthcare, and palliative care.
3. Pradhan Mantri National Dialysis Programme (PMNDP): Since its launch in 2016, this program has helped 2.5 million poor patients access dialysis services, alleviating a significant financial burden on disadvantaged groups.
4. Pradhan Mantri Bhartiya Janaushadhi Pariyojana (PMBJP): A scheme designed to make affordable generic medicines accessible to the public. By 2024, this initiative had significantly expanded, leading to household savings of thousands of crores of rupees.
Challenges in Health Financing:
While India’s health financing landscape has undergone a significant transformation, several challenges remain. These include:
1. Maintaining Public Health Spending: Both state and union governments must ensure that the momentum in health spending continues. Health is primarily a state subject, and while fiscal devolution has increased the funds available to state governments, these funds have not always translated into higher healthcare spending. For example, fiscal devolution from 32% during the 13th Finance Commission to 42% during the 14th Finance Commission did not lead to proportional increases in health expenditure at the state level.
2. Unspent Allocations: Despite the pandemic-triggered surge in health budgets, a significant portion of union government allocations remains unspent. This highlights issues in fund utilization and calls for improved administrative capacities to absorb and deploy funds effectively.
3. Quality of Care and Continuum of Services: Ensuring the quality of medicines remains a challenge, as cases of spurious drugs entering public supply chains still occur. Additionally, the integration of secondary and tertiary care provided through AB-PMJAY with primary care offered by AAMs is crucial to create a continuum of care. Without this integration, many patients continue to face difficulties navigating the healthcare system.
4. Rare Diseases and Population-Specific Needs: While AB-PMJAY and AAMs address a wide range of health issues, policies targeting rare diseases and other under-represented health needs are still lacking. These gaps need to be filled to ensure equitable healthcare access for all segments of the population.
The Way Forward:
India's health system has seen considerable improvements over the last decade, particularly in reducing OOPE and expanding public health services. However, the country still has a long way to go. Sustained government investment in health, along with better fund utilization and integration of healthcare services, will be essential for India to meet the NHP 2017 target of 2.5% of GDP in public health spending by 2025.
Looking ahead, it is critical for both the union and state governments to focus on:
· Maintaining and increasing health budgets.
· Enhancing administrative capacities for better utilization of allocated funds.
· Ensuring continuum of care by integrating primary, secondary, and tertiary services.
· Addressing gaps in quality control and population-specific health needs.
India has the potential to become a global example of successful health financing reforms. However, this will require continued focus, political will, and sustained investment in the health sector. Health security has emerged as a critical pillar of national security, as underscored by the COVID-19 pandemic. Investing in health is not just a social imperative but also an economic necessity for the country’s future.
|
Probable questions for UPSC Mains exam: Health security is now considered a critical pillar of national security. Analyze how investing in healthcare is not only a social imperative but also an economic necessity for India's long-term development. |








