Introduction
Anemia remains a significant public health challenge in India, where it disproportionately affects women, children, and adolescents. Despite being preventable and treatable, anemia continues to persist due to multifaceted causes such as nutritional deficiencies, environmental factors, and inadequate healthcare access. Iron deficiency is the primary cause of anemia, though deficiencies in folate, vitamin B12, and vitamin A also play a crucial role. The condition manifests as fatigue, dizziness, and shortness of breath, often signaling deeper nutritional and health issues.
Although India has made progress in improving its healthcare system, the prevalence of anemia remains alarmingly high. Factors such as poor dietary intake, early pregnancies, inadequate maternal care, and limited access to iron-rich foods continue to fuel the epidemic. In response, the Government of India has implemented several interventions, most notably the Anemia Mukt Bharat (AMB) campaign. However, new research has revealed a more complex picture, urging a reevaluation of existing policies.
A nationwide study (2016–2018) and a 2025 publication in the European Journal of Clinical Nutrition revealed that iron deficiency accounts for less than one-third of anemia cases. Vitamin B12 and folate deficiencies, along with environmental factors like air pollution, are now recognized as significant contributors.
Understanding Anemia: Symptoms, Impact, and Vulnerable Groups
Anemia occurs when there is insufficient hemoglobin in the blood to carry oxygen effectively, leading to symptoms such as fatigue, light-headedness, cold extremities, and reduced physical endurance. The condition affects several vulnerable groups, including:
- Children under five, particularly those below two years of age
- Adolescent girls and women
- Pregnant and postpartum women
Iron deficiency anemia in children can significantly hinder cognitive and motor development, while in adults, it reduces productivity. In pregnancy, anemia increases the risks of low birth weight, preterm delivery, and perinatal mortality.
Global and National Burden of Anemia
Anemia is a global health crisis. In 2019, approximately 500 million women aged 15–49 years and 269 million children under five were anemic. Among women, 30% of non-pregnant women (around 539 million) and 37% of pregnant women (approximately 32 million) suffered from anemia.
In India, the National Family Health Survey-5 (2019–2021) highlighted a persistent burden of anemia, particularly among women and children. Despite decades of nutrition-focused interventions, the prevalence of anemia has either stagnated or worsened in many demographic groups, including women of reproductive age, adolescents, and the elderly.
Anemia can result from various factors beyond iron deficiency, including:
- Deficiencies in vitamin B12, folate, vitamin A, D, and zinc
- Chronic conditions such as kidney disease, rheumatoid arthritis, and cancer
- Infections like malaria and tuberculosis, particularly in economically disadvantaged populations
- Environmental factors, especially air pollution
Anemia due to air pollution and other factors:
Research has shown that anemia is often multifactorial, and iron-centric treatment policies are insufficient. Only 25–30% of anemia cases can be resolved through iron supplementation. As a result, addressing anemia requires a more comprehensive, multidimensional approach.
One key factor emerging from studies is air pollution. Research has found that a 10 µg/m³ increase in fine particulate matter (PM 2.5) exposure correlates with a 10% rise in anemia among children and 7.2% among women of reproductive age. Pollutants like PM 2.5 trigger the production of cytokines, which in turn increase the liver’s production of hepcidin, a hormone that inhibits iron absorption. Air pollution also suppresses bone marrow activity, reducing red blood cell production.
Given that India experiences widespread exposure to unhealthy PM 2.5 levels, addressing air pollution could significantly reduce anemia prevalence. For example, meeting India’s clean air targets could reduce anemia rates among women of reproductive age to 39.5%, bringing 186 districts below the national target of 35%.
Policy Interventions in India:
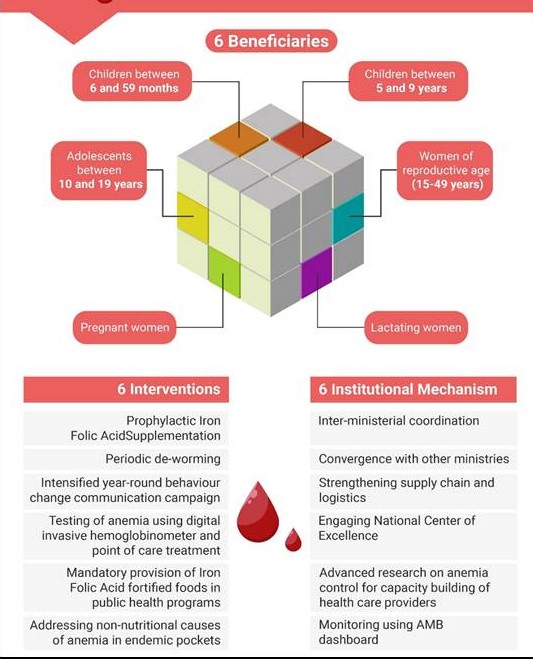
The Government of India’s Anemia Mukt Bharat (AMB) program, launched in 2018, is a comprehensive effort to address the anemia crisis. It adopts a 6x6x6 strategy, focusing on six priority groups, implementing six interventions, and involving six institutional mechanisms. The targeted groups include:
1. Preschool children (6–59 months)
2. Children (5–9 years)
3. Adolescents (10–19 years)
4. Pregnant women
5. Lactating mothers
6. Women of reproductive age (15–49 years)
Key interventions under AMB include:
1. Prophylactic Iron and Folic Acid Supplementation (IFA):
o Biweekly IFA syrup for children (6–59 months)
o Weekly IFA tablets for school-age children, adolescents, and women
o Daily supplementation for pregnant and postpartum women
2. Biannual Deworming Campaigns: These are conducted during National Deworming Days in February and August, extending services to pregnant women during ANC visits.
3. Behavior Change Communication Campaign: The “Solid Body, Smart Mind” campaign promotes key behaviors like nutrition, sanitation, deworming, and IFA adherence.
4. Point-of-Care Testing and Digital Treatment Tools: Emphasis on accessible testing and timely treatment, especially for school-going adolescents and pregnant women.
5. Mandatory Provision of Fortified Foods: Integration of iron- and folic acid-fortified food in all government-funded nutrition programs.
6. Addressing Non-Nutritional Causes: Screening and treating conditions like malaria and fluorosis in endemic areas.
These interventions are supported by pre-existing platforms like the National Iron Plus Initiative (NIPI) and Weekly Iron and Folic Acid Supplementation (WIFS), aligned with the National Health Mission (NHM).
Limitations of Current Fortification Policies
While the AMB program promotes iron and folic acid supplementation and fortified rice in public food distribution systems, these efforts face significant challenges. Universal iron fortification does not address other causes of anemia, and excessive iron intake can lead to health issues like diabetes—a growing concern in India, where 101 million people are diabetic.
Additionally, the grain-centric food policy limits dietary diversity, exacerbating nutritional deficiencies. Experts like Kurpad advocate for a shift toward horticulture-based nutrition, ensuring affordable access to fruits and vegetables that offer broader health benefits.
Improving Bioavailability:
Iron absorption is influenced by dietary factors. Vitamin C enhances iron absorption by up to 25% when consumed alongside iron-rich foods, while inhibitors like phytates, tannins (found in tea/coffee), and calcium block this absorption. A study in rural Haryana (2024) showed that adding guava to a mung bean-based school meal significantly reduced anemia prevalence, highlighting the importance of combining iron with vitamin C-rich foods.
Challenges in Awareness and Behavioral Change
Anaemia is also an awareness issue. Many individuals discontinue supplements due to side effects like constipation. Experts stress the need for mass awareness campaigns, community involvement, and engagement through public figures to promote anemia education. Without broad community support, even well-designed strategies may fail in the long term.
Conclusion
Anemia, a complex condition influenced by nutrition, environment, chronic disease, and social awareness, demands a comprehensive and holistic public health strategy. Addressing it requires more than just food-based solutions. By integrating environmental reforms, dietary diversity, targeted supplementation, and robust community engagement, India can effectively reduce anemia prevalence.
| Main Question: Evaluate the effectiveness of the Anemia Mukt Bharat (AMB) program in addressing the anemia crisis in India. What additional measures would improve its implementation? |