Non-communicable diseases (NCDs) such as diabetes, cardiovascular diseases, cancer, and stroke are rapidly emerging as significant public health challenges in urban India. Recent incidents, like the cardiac arrest and subsequent death of a Bengaluru Metropolitan Transport Corporation (BMTC) bus driver, underscore the urgency of addressing this growing health crisis. The complexities of urban life, coupled with socio-economic disparities, necessitate a robust and inclusive response to curb the rising burden of NCDs.
Why is This Issue Critical?
Urbanization and Health Challenges
- Urbanization has significantly altered lifestyles, with more than 50% of the global population living in urban areas—a figure projected to rise to 70% by 2050.
- In India, urban centers host a diverse population, including approximately 41 million inter-state migrants (Census 2011), many of whom live in substandard housing and face limited access to healthcare.
- Nearly 49% of urban dwellers in India live in slums or informal settlements (UN-Habitat/World Bank, 2022), where access to healthcare and sanitation is inadequate.
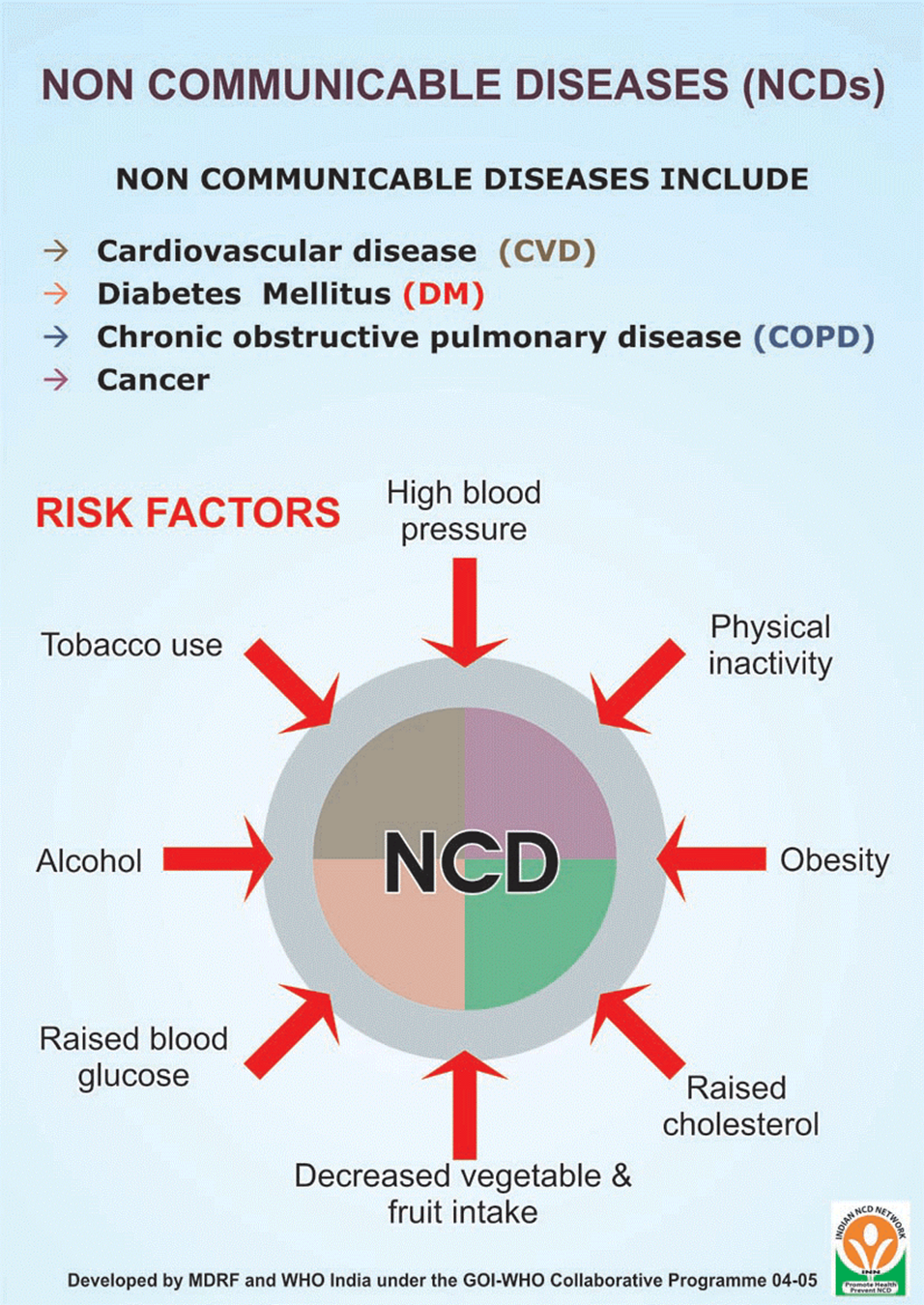
The Rising Burden of NCDs
- Data from the National Family Health Survey (NFHS) shows a marked increase in hypertension, diabetes, and obesity among urban populations.
- India has witnessed a threefold rise in NCD prevalence since 1995, creating a dual burden alongside persistent infectious diseases.
- NCDs often develop silently, highlighting the need for regular health screenings and early interventions.
Factors Responsible:
High-Stress Work Environments
- Urban workers, particularly in professions like transportation and sanitation, face excessive stress due to long hours, erratic schedules, and challenging working conditions.
- A study of BMTC employees revealed that over 40% of workers aged 45-60 are at high risk for cardiovascular diseases, exacerbated by continuous driving and poor eating habits.
Poor Nutrition and Sedentary Lifestyles
- Access to nutritious food and opportunities for physical activity is limited, especially among low-income urban populations.
- The prevalence of fast food, coupled with sedentary lifestyles, contributes significantly to obesity, hypertension, and diabetes.
Socioeconomic Marginalization
- Many urban residents, particularly those in slums and informal settlements, lack access to quality healthcare and health insurance.
- Financial constraints often lead to delayed diagnoses and inadequate treatment, worsening health outcomes.
Inadequate Awareness and Screening
- Many individuals are unaware of the importance of regular health checkups and preventive care.
- Insufficient screening facilities and lack of community-level health programs hinder early detection of NCDs.
Challenges in Urban Health Systems
Limited Accessibility and Overburdened Infrastructure
- Public healthcare facilities in urban areas are often overcrowded, while private healthcare remains unaffordable for many.
- The lack of healthcare services in slums and informal settlements leaves vulnerable populations underserved.
Financial Vulnerability
- High out-of-pocket (OOP) healthcare expenditure places a significant financial burden on families, particularly those living near or below the poverty line.
- Informal workers, who often lack health insurance, are at greater risk of catastrophic healthcare costs.
Fragmented Service Delivery
- The absence of a cohesive and integrated healthcare system in urban areas results in inefficient service delivery and poor health outcomes.
Strengthening Urban Health Systems
Expanding Primary Healthcare Services
- Establish more primary healthcare centers in underserved areas to improve accessibility.
- Focus on affordable and culturally appropriate healthcare for low-income populations.
Implementing Regular Health Screenings
- Mandate regular health evaluations for high-risk groups, including transport workers, sanitation staff, and gig economy employees.
- Early detection of risk factors like high blood pressure and blood sugar levels can prevent severe complications.
Integrating Health with Employment Policies
- Employers should collaborate with health departments to provide wellness programs, including stress management workshops, nutrition counseling, and fitness initiatives.
- Extend health insurance coverage to informal and contractual workers, ensuring access to essential medical care.
Leveraging Technology in NCD Management
Real-Time Health Monitoring
- Digital tools like mobile apps and wearable devices can enable continuous monitoring of health metrics, allowing for early intervention in conditions like hypertension and diabetes.
- Technology-driven solutions can improve outreach and engagement in underserved communities.
Raising Awareness through Digital Platforms
- Use social media campaigns and digital tools to educate the public about NCD prevention and healthy lifestyle choices.
- Telemedicine services can bridge gaps in access to healthcare, particularly for marginalized urban populations.
The Role of Community Engagement
Health Promotion Campaigns
- Conduct public awareness campaigns emphasizing the importance of regular health screenings and preventive care.
- Promote healthy lifestyle choices, such as balanced diets, regular exercise, and smoking cessation.
Community-Led Initiatives
- Empower local organizations to conduct workshops and outreach programs tailored to community needs.
- Foster partnerships between healthcare providers, local governments, and community groups to co-create solutions.
Building Support Networks
- Create peer support groups to address shared challenges and encourage collective action.
- Community networks can play a crucial role in promoting health education and resource sharing.
The Way Forward
Policy Recommendations
1. Strengthen Urban Healthcare Infrastructure
o Expand the reach of primary healthcare centers in urban slums and underserved areas.
o Invest in mobile health units to provide services to populations with limited access.
2. Promote Preventive Care
o Mandate regular health screenings for vulnerable groups, ensuring early detection of risk factors.
o Increase awareness campaigns targeting specific urban challenges, such as sedentary lifestyles and poor nutrition.
3. Integrate Health with Employment
o Employers should implement wellness programs that include regular screenings, nutrition counseling, and fitness initiatives.
o Extend mandatory health insurance coverage to informal sector workers.
4. Leverage Technology
o Utilize digital tools for health monitoring, public awareness campaigns, and telemedicine services.
o Develop health apps tailored for low-income populations to encourage regular checkups and lifestyle improvements.
5. Foster Community Partnerships
o Encourage local organizations to lead health promotion campaigns and organize screening camps.
o Empower communities to take ownership of their health outcomes through participatory programs.
Conclusion
The rising burden of non-communicable diseases in urban India calls for immediate, multi-faceted interventions. Strengthening healthcare infrastructure, integrating wellness programs with employment policies, leveraging technology, and fostering community engagement are critical to addressing this crisis. Collaborative efforts among policymakers, healthcare providers, employers, and communities can pave the way for healthier, more resilient urban environments. By prioritizing prevention, early detection, and equitable access to healthcare, India can ensure a brighter and healthier future for its urban population.
|
Probable questions for UPSC Mains exam: Examine the socio-economic factors that contribute to poor health outcomes in urban informal settlements. Suggest measures to strengthen urban healthcare systems to address these challenges. |